What To Expect
What to Expect
Your anesthesia experience includes three components:
Preoperative
Safety First – Before your surgery, your anesthesiologist will consult with the surgical team preparing you to more safely undergo your planned procedure. On occasion, your evaluation may elicit a new medical problem or determine that your current medical problems require further investigation and treatment prior to surgery. We want you to undergo your surgery safely and it is important for you to be forthcoming about your medical history, and complete any required testing prior to your procedure.
Another important preoperative requirement is to strictly follow any fasting directives. These have been put in place for your own safety. Eating a full breakfast for example and not informing your anesthesiologist will put you at grave risk for “aspiration pneumonitis,” in which any food in your stomach can come up your esophagus and travel into your lungs, potentially causing serious lung damage. Remember, your anesthesiologist wants you to get through your surgery safely. Please diligently follow all of your preoperative instructions including the use of only authorized medications and supplements prior to your surgery.
Intraoperative
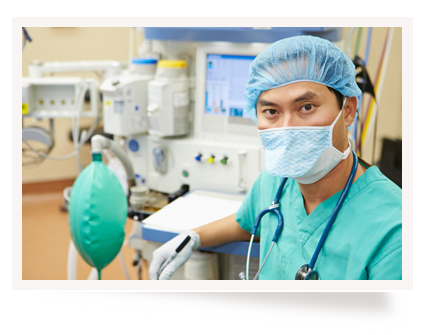
Quality Monitoring During surgery, your anesthesia care team will be by your side for the entire time you are under anesthesia. They continuously monitor your vital functions, including your pulse, blood pressure, oxygen level, ventilation (breathing) and level of anesthesia. On occasion your anesthesia care team will perform additional procedures to more closely monitor your blood pressure or your heart function depending on your medical condition and type of surgery. In addition, your anesthesia care team keeps a close eye on your fluid status and administers any necessary intravenous fluids or blood and blood products during your surgery. We will also administer any required pain medication and anti-nausea medication before you leave the operating room.
Some patients are concerned about “waking up” during their surgery. Your anesthesia care team will continuously monitor not only your vital signs, but your “depth” of anesthesia to minimize the risk of any intraoperative awareness. In addition we frequently utilize a special device that monitors your EEG, or brain function, confirming that you are indeed asleep.
Post-Operative
Special Care – After your surgery, your anesthesia care team will personally transport you to a post anesthesia care unit (PACU), a specialized recovery room, where registered nurses with extensive training or ICU (intensive care unit) experience will closely monitor your vital signs. You may be somewhat drowsy and confused when you first wake up. When you meet certain discharge criteria your anesthesiologist will medically discharge you to your own room or to a waiting area prior to discharge if you are an outpatient.
If you experience any pain or nausea after waking up, it is important to quickly inform your R.N. On occasion, despite our best efforts, some patients (who are more prone to nausea) will still get nauseated after surgery. If this happens we will aggressively treat your symptoms with the help of our PACU nurses. Some patients must be kept be kept on a breathing machine or ventilator after the procedure due to the type of surgery (e.g. open heart surgery) or due to your medical condition (e.g. severe lung disease). In that situation, your anesthesiologist will transport you to the PACU or ICU sedated and order medication for your comfort as you awaken.

Videos: Anesthesia and You
This two-part video series tells you who an anesthesiologist is, what an anesthesiologist does, and how the anesthesiologist is your lifeline to modern medicine before, during and after surgery. We encourage you to watch both of these videos and make a note of any questions you may have, then bring them to your next physician visit or when you meet with your anesthesia care team before surgery.
Part 1:
Part 2:


